Why conformance is key to secure, connected and consumer-centred care

The future of digital health is not just approaching the horizon; it is already here. In the context of the Sharing by Default to My Health Record initiative, the Australian Digital Health Agency’s Chief Clinical Adviser (Nursing) sets out why it’s time for secure and seamless health data exchange — and an emergency physician provides a supportive case study.
In health care, accurate and timely information can mean the difference between effective treatment and avoidable complications. It can even be the difference between life and death. As a nursing professional, I have seen firsthand the challenges that arise when vital patient information is inaccessible. Nurses, often the frontline providers of patient care, rely heavily on accurate data to make informed decisions, administer medications safely and monitor patient progress. Yet, for decades, Australia’s healthcare system has relied on outdated information-sharing models, where consumer data is locked in disconnected silos, accessible only to a select few. This approach, once acceptable in an era of filing cabinets and fax machines, no longer serves modern healthcare needs.
I view the transition of traditional healthcare information like an old-fashioned key and lock system. Imagine consumers having multiple keys, each one granting access to different parts of their health information, stored in separate locked cabinets. If a new healthcare provider joins their care team, they would need to acquire all the specific keys to unlock the needed information. In contrast, modern digital health acts like a personal safe deposit box for the consumer. They hold the master key, giving them the power to control who can access their health data, ensuring it is always within reach for healthcare providers involved in their care.
This centralised repository allows for seamless sharing and retrieval of all pertinent information, making sure no critical detail is overlooked or inaccessible. As consumers’ healthcare needs evolve, they retain control over their data, ensuring timely and secure access for their dynamic care team. Of even greater importance is that consumers use their health information to help inform choices about their own care.
A turning point in the transformation of health care
The future direction of health care is at a crossroads, where technology must evolve to match consumer expectations. Australians now expect their health data to be in their control and available when and where they need it, just as they expect instant access to banking, travel and communication tools. The federal government’s Sharing by Default to My Health Record initiative marks a major turning point in delivering secure, real-time interoperability, ensuring that health information is consumer-controlled, discoverable, accessible and shareable between healthcare providers involved in their care. Legislative changes will ensure key health information, starting with the upload of pathology reports and diagnostic imaging results by default to My Health Record, will empower consumers to take charge of their key health information and allow healthcare providers to access real-time data. This is an opportunity that is as critical as it is exciting.
This crucial sharing of information reminds me of a conversation a colleague once had with an emergency nurse on the importance of having real-time patient data. They described an emergency situation when they spent half an hour calling radiology providers to see if they were “the blue place around the corner from a servo” that a distressed patient described as having a critical scan result. They agreed it was time that could have been better spent with the patient.
For me, the benefits of interoperability in a hospital setting are clear. Consider, for example, an unconscious patient in the emergency room with no one else present to provide their medical history. Healthcare providers on the front line waste precious minutes chasing down scattered medical records, hoping to piece together a life-saving treatment plan. They may be unable to determine whether the patient has allergies, chronic illnesses or medications that could interact dangerously with emergency treatment. With information going into My Health Record by default, this can be retrieved as soon as the patient’s identification is confirmed, allowing healthcare providers to make clinical decisions with more confidence. The time spent hunting for old results will be a thing of the past.
A framework for secure and seamless data exchange
While it’s important to continue supporting processes that help vulnerable and less digitally connected Australians, there are a growing number of people who are increasingly digitally savvy and expect seamless, user-friendly digital health solutions. They want access to their health information to make better choices about their health and care. Undoubtedly, this expectation presents many challenges, as the industry grapples with privacy concerns, cybersecurity risks, and the overarching responsibility of ensuring that health data remains secure and trusted.
At the Australian Digital Health Agency (the Agency), these challenges are taken seriously and managed through a Conformance Framework which ensures that digital health tools meet rigorous security standards, protecting consumer privacy while enabling seamless data exchange. It outlines the processes through which healthcare organisations and their software vendors can assess and demonstrate their alignment with the national standards. The specifications outlined in the Conformance Framework detail conformance profiles that show how software must behave to ensure data is managed securely, safely, and in line with legislative and policy expectations.
A conformance profile is like a checklist that shows whether a digital health system follows specific technical standards. It helps ensure that different systems can safely and reliably share information with each other by using standard language, rules and behaviours.
While the rules that underpin the Sharing by Default legislation are still being finalised, there is no doubt that existing conformance processes will be leveraged and strengthened. This will help the sector adapt to the new requirements without compromising the safety and security of consumer information.
As Sharing by Default expands, it is not just higher data volumes that drive the need to update conformance profiles — it is also about ensuring we remain at the forefront of digital health innovation. When profiles are updated, it’s vital to guide the sector through the changes, including setting an expiry, or sunset date, on older conformance profiles. The Agency collaborates closely with developers to ensure systems are up to date.
Shaping the future of digital health for all Australians
Digital health is not solely about efficiency; it’s also about equity. A truly connected healthcare system ensures every Australian, regardless of location or circumstance, has access to the same high-quality care. As the capabilities of My Health Record expand, the Agency is co-designing these solutions with consumers, healthcare providers, software vendors and policymakers, because a modern healthcare system is only effective if it is trusted, accessible and built for the people it serves.
As digital health leaders, we must do more. Our role is to ensure the sector is not only prepared for the coming change but actively shaping it. We must align incentives, enforce conformance and, most importantly, protect the trust Australians place in our health system. The real measure of success won’t be gauged by ‘system uptime’ or ‘authentication compliance’, but by situations like when an emergency nurse can instantly access the right scan at the right time to make a potentially lifesaving decision. That is what digital health can and must deliver. That is the promise of Sharing by Default, founded on conformance requirements that make information-sharing secure, valuable and dependable for all Australians.
The future of digital health is not just approaching the horizon; it is already here. It’s time to remove the silos that prevent connected care. It is our responsibility to ensure that every consumer, provider and policymaker is ready for it.
This shift towards more digitally enabled models of care also highlights the importance of a skilled, adaptable workforce. Attracting and developing digital capability across health professions is critical to sustaining innovation and ensuring long-term system resilience. The Agency works with universities, research institutions and professional bodies to embed digital health competencies into medical, nursing and allied health education. By modernising training and showcasing the role of digital tools in improving care, we can help make health professions more appealing to the next generation and strengthen Australia’s position in digital health leadership.

**************************************************
Author spotlight
Karen is an influential leader who has been advocating for the role of nurses in digital health for many years. She has been a key contributor to the advancement of digital health in the nursing profession and played a pivotal role in the future of the Australian healthcare system as a member of the Strengthening Medicare Taskforce and has participated in numerous national health policy advisory groups, including providing advice to the Primary Health Care Advisory Group, the MBS review and Primary Health Reform Steering Group for the National Primary Health Care 10 Year Plan.
**************************************************
A supportive case study
Lost in the system: solving the mystery of missing patient data
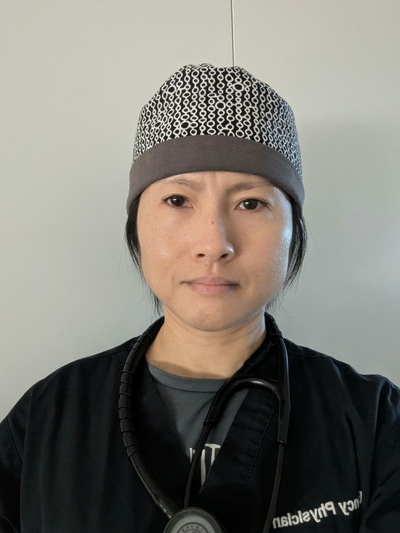
The frequent challenge in Emergency Medicine is seeking out relevant patient information in a fragmented healthcare system short on time and resources.
Sometimes, you need the detective skills of Sherlock Holmes to solve the mystery of where and when the patient had their last investigations done. Hunting down these records can often involve phoning multiple providers in the search for clues to the missing data.
Trying to hunt down patients’ results sometimes involves working out where they even had the investigations done and phoning multiple possible providers. This wastes time that would be better spent providing actual clinical care to the patient, or to the many other patients still waiting to be seen. Unfortunately, this is not a task we can delegate to administration staff.
More difficulties arise because people often present to the ED outside of typical business hours, when they are unable to access their usual healthcare providers. This means that the GP clinics they attend are not available for us to contact for health summaries or important investigation results. Many private radiology providers also have no after-hours options for us to get results.
If doctors send patients to hospital because of abnormal pathology results, we will often repeat pathology in the ED to exclude a false result before starting treatment.
However, we still need to know what the abnormal result was. There have been many occasions where the patient does not even know what result was abnormal. They simply say that their doctor phoned and told them to go to Emergency.
We usually also need to know what a patient’s previous pathology results were to have a baseline comparison. If a patient has impaired renal function on blood tests in Emergency, our approach differs if this is new for them, as opposed to if it is normal for them due to a chronic condition. It can mean needing a host of extra tests and hospital admission or alternatively being able to discharge someone.
Sometimes, patients present with ongoing symptoms that have already been recently investigated by their usual healthcare providers. Take, for example, a patient with abdominal pain who has had a CT just a few days ago for the same symptoms. Attempts would usually be made to try to obtain that result rather than repeat the CT, to avoid exposing the patient to unnecessary radiation. What that has sometimes meant, when the radiology provider was uncontactable for the result, was that we had to keep the patients in Emergency overnight until the provider was available in “business hours”. This has flow-on impacts for ED capacity, affecting available space to see other patients.
To avoid errors, it is vital to have a copy of the result, rather than just a report over the phone. However, there is often a delay in having results sent through (usually faxed, less commonly emailed) after we have managed to contact the external investigation providers. This can mean multiple subsequent follow-up phone calls to chase up results that have not arrived as expected.
Having near real-time access to patient investigation results would provide us with a faster and more accurate picture of the patient’s condition so we can determine next steps. This means patients would avoid having to wait extra hours in Emergency for us to get results, which has benefits for not only the individual patient, but the efficiency of the entire system. It will mean physicians such as myself can go back to doing what we do best, providing emergency health care, and we can leave the detective work to the likes of Sherlock Holmes.
**************************************************
**************************************************
In Conversation with Australasian Institute of Digital Health CEO Anja Nikolic
Hospital + Healthcare speaks with Australasian Institute of Digital Health CEO Anja...
Cutting-edge digital health tools putting plastic, silicon and steel to the sword
The Australian Digital Health Agency's Chief Digital Officer sets out some sustainable...
How are AI models approved for use in health care?
Hospital + Healthcare speaks with the Therapeutic Goods Administration to...

![[New Zealand] Transform from Security Awareness to a Security Culture: A Vital Shift for SMB Healthcare — Webinar](https://d1v1e13ebw3o15.cloudfront.net/data/89856/wfmedia_thumb/..jpg)
![[Australia] Transform from Security Awareness to a Security Culture: A Vital Shift for SMB Healthcare — Webinar](https://d1v1e13ebw3o15.cloudfront.net/data/89855/wfmedia_thumb/..jpg)




