Doctors at breaking point — can AI medical scribes help?

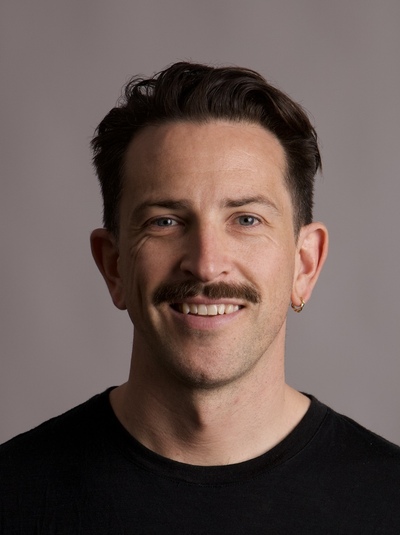
A former frontline medical doctor — who, following burnout, now works as a go-to-market clinical specialist for an AI medical scribe provider — sets out how AI scribes might be able to help hospital health practitioners.
Australia’s healthcare system has reached breaking point. Hospitals are underfunded, clinicians are overwhelmed, wait times are blowing out and patients are paying the price. Without significant intervention and innovation, this trend will continue to worsen. Research by the Australian Health Practitioner Regulation Agency shows that 12% of health practitioners are either doubting their profession or intending to leave, with most intending to do so within the year.1
It comes as Australia’s population both grows and ages, putting even greater burden on a sector where healthcare professionals are being asked to do more with less every year. Burnout, unfulfilling work, and lack of satisfaction and job security are among the top reasons practitioners intend to leave the profession. Meanwhile, fulfilment, work-life balance and doing the work they were trained to do tops the list of reasons to stay. We must find ways to reduce the drivers of attrition while maximising the reasons clinicians choose to stay.
The risks to Australia’s healthcare system
Like most who enter the profession, I was driven by a simple but powerful motivation: I wanted to help people. That simple desire set me on a path that included eight years of university study, then six years of training as a doctor in surgical and then critical care settings. However, like thousands of my peers, the burden became too much, and I left frontline medical care in 2023; burnt out and disenfranchised with a system that fails its staff consistently.
I’m not alone; according to research from the Australian Journal of General Practice, burnout is common in primary care doctors.2 As Australia’s population grows, and our healthcare needs become more complex, the burden on an already-overstretched healthcare fraternity will increase. If clinicians continue to leave the sector at the same unsustainable rate, or if the growth of the sector doesn’t match the growth of our population and its healthcare needs, wait times will worsen, consultations will be rushed and the risk of error will increase exponentially.
What’s more, as clinicians leave the sector, hospitals will be forced to rely more on costly locum staff or burn out existing teams, both of which are unsustainable and short-sighted, especially as conversations around funding continue to intensify. If clinicians exit mid-career, it creates a drain of experienced professionals and mentorship gaps for junior doctors. The clinical and practical knowledge that these professionals possess — from nuanced diagnostic insights to navigating complex patient care scenarios — is lost, leaving junior doctors without the guidance they need to develop confidently and competently early in their careers.
Using technology to restore purpose and improve the quality of care
A 2022 UK report revealed that NHS clinicians spend one-third of their working hours on generating clinical documentation, 25% more than seven years before.3 We didn’t pursue a career in medicine to sit behind a screen or be buried in notes for half the day. While documentation is an occupational necessity, it has spiralled out of control of late. By reducing the administrative burden of clinicians, we can return them to the patient-facing work that is most likely to keep them in the profession.
Technology, such as AI medical scribes, frees clinicians from administrative burden, so they can focus on care, not paperwork. By ambiently transcribing patient consultations, once consent from the patient has been granted, clinicians can save up to two hours every single day. From GPs to emergency doctors, that’s a day of work saved every single week. Typically, GPs have overbooked clinics and stay after hours to catch up on notes at the end of each session. However, with AI much of this burden is automated over the course of the day, so GPs are not spending extended periods of time at the end of a shift catching up on admin tasks to get patients the care they need.
In a ‘fast track’ ED treating, for example, minor injuries, fractures and wounds, AI enables a doctor to move onto a new patient within minutes, rather than spending 10–15 minutes writing notes between each patient. In resus and acute areas, where patients are more critically unwell and have more nuanced cases, clinicians can save 20 minutes during a one-hour consultation. Most importantly, their treating team can spend more time with these patients, rather than being at a computer as a result.
The Australian Government’s Productivity Commission has identified AI as a major priority, and is of the view that the technology will have a substantial impact on productivity.4 In few instances and in few sectors could the benefits be greater than in health care. However, to feel these benefits, more investment is needed, as are formal frameworks to unlock its potential. Ultimately, if successful, we can save clinicians time and help them return to what inspired them to pursue the profession in the first place: diagnosing, treating and building patient relationships.
The potential of AI
Health care at its core will always be about delivering human-centred care. Increasing administrative burden and relentless workloads continue to push doctors to spend less time at the patient’s bedside delivering care. We must give clinicians all the tools to do their job. Deploying AI to reduce administrative workload and returning their focus on delivering care is an obvious solution — one that makes us better placed to reduce the burden on doctors, ease the drain from the sector, and improve the quality and quantity of patient care delivered every day.
Though they offer a potential solution to help clinicians manage administrative tasks, AI scribes are not replacements for clinical judgement. The Australasian Institute of Digital Health has recently released an information sheet — ‘Implementation of AI scribes in healthcare workflows’ — designed to be a comprehensive guide for clinicians, practice managers and digital health leaders. You can access it at digitalhealth.org.au/new-resource-ai-scribes-in-australian-healthcare.
1. Tan J, Divakar R, Barclay L, Bayyavarapu Bapuji S, Anderson S, Saar E. Trends in retention and attrition in nine regulated health professions in Australia. Aust Health Rev. 2025;49:AH24268. doi: 10.1071/AH24268
2. Toukhsati SR, Kippen R, Taylor C. Burnout and retention of general practice supervisors: prevalence, risk factors and self-care. Aust J Gen Pract. 2024;53(12 Suppl):S85–S90. doi: 10.31128/AJGP-11-23-7011
3. Nuance Communications Ireland, Ltd. Assessing the burden of clinical documentation. October 2022. [Internet]. https://www.nuance.com/asset/en_uk/collateral/enterprise/report/rpt-assessing-the-burden-of-clinical-documentation-en-uk.pdf
4. Productivity Commission. Senate Select Committee on Adopting Artificial Intelligence (AI): Productivity Commission submission. 2024. [Internet] Canberra (AU): PC;2024. https://www.pc.gov.au/research/supporting/adopting-artificial-intelligence/adopting-artificial-intelligence.pdf
In Conversation with Australasian Institute of Digital Health CEO Anja Nikolic
Hospital + Healthcare speaks with Australasian Institute of Digital Health CEO Anja...
Cutting-edge digital health tools putting plastic, silicon and steel to the sword
The Australian Digital Health Agency's Chief Digital Officer sets out some sustainable...
How are AI models approved for use in health care?
Hospital + Healthcare speaks with the Therapeutic Goods Administration to...

![[New Zealand] Transform from Security Awareness to a Security Culture: A Vital Shift for SMB Healthcare — Webinar](https://d1v1e13ebw3o15.cloudfront.net/data/89856/wfmedia_thumb/..jpg)
![[Australia] Transform from Security Awareness to a Security Culture: A Vital Shift for SMB Healthcare — Webinar](https://d1v1e13ebw3o15.cloudfront.net/data/89855/wfmedia_thumb/..jpg)




