The device set to reform stroke care for all Australians
Scott Kirkland is Co-Founder and Executive Director at EMVision, a healthcare technology company aiming to change the stroke care paradigm. EMVision has developed a portable brain scanner for rapid, point-of-care stroke diagnosis and monitoring, which is set to transform stroke care, particularly for Australians living in regional areas, who are 17% more likely to suffer a stroke than those in metropolitan areas, and often unable to access specialised care. There is a critical need to narrow the gap in stroke care between Indigenous and non-Indigenous Australians living in regional areas, with First Nations Peoples having close to three times the rate of acute ischemic stroke incidence and mortality.
Kirkland told Hospital + Healthcare about the company’s mission to provide equal access to healthcare, how EMVision’s technology is set to transform stroke care and diagnosis for rural/regional Australians, and why we need to act urgently.
What factors contribute to the higher rate of stroke and poorer stroke outcomes outside metropolitan areas?
For stroke outcomes, time is everything. The best outcomes are achieved when a patient is treated in the first few hours after stroke onset, ideally within the ‘golden hour’. The tyrannies of distance play a significant role here. Unfortunately, only 3% of patients in rural and remote areas of Australia are treated in a stroke unit, compared with 77% of patients in metropolitan areas. In fact, most rural and remote patients need to travel more than 200 kilometres to access care.
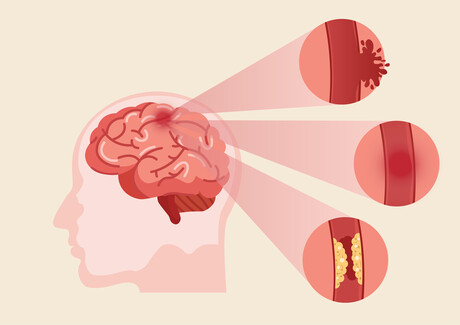
Stroke is highly treatable but requires access to urgent neuroimaging first to help health practitioners accurately diagnose and treat the condition.
Taking away the urban/regional factor, is there a marked difference in stroke rates between Indigenous Australians and non-Indigenous Australians in regional areas and, if so, what are the main reasons for this?
There are unacceptable disparities in stroke outcomes between Indigenous Australians and non-Indigenous Australians. Indigenous Australians are twice as likely to be hospitalised with stroke and 1.4 times as likely to die from stroke than non-Indigenous Australians. Of additional concern, life expectancy for Indigenous Australians is already 10 years shorter.
The Stroke Foundation’s National Audit of Acute Services found that Indigenous patients have a greater prevalence of stroke risk factors, such as diabetes — more had intracerebral haemorrhages, and were less likely to be treated in a stroke unit than non-Indigenous patients.
What steps are being taken to address rates of stroke in regional areas and for Indigenous communities?
Earlier this year, the Australian Stroke Alliance (ASA) — which is working with Aboriginal and Torres Strait Islander communities as well as Indigenous health experts — was awarded a $40 million Medical Research Fund grant to tackle these challenges, in partnership with EMVision.
Through the ASA program, we’ll adapt our lightweight and affordable portable brain scanner technology for road ambulances and air deployment with the Royal Flying Doctor Service, which paired with a national telehealth platform, will help enable all Australians to receive time-critical stroke care, regardless of their location.
More recently, the federal government announced a further $180 million in medical research funding and investment to tackle stroke. This investment will support home-grown research into cardiovascular health, from real-time cardiac monitoring to after-stroke care for Aboriginal and Torres Strait Islander patients.
It’s clear that improving stroke outcomes and reducing the huge health economic burden is top of mind for our federal government.

Can you provide more details about the neuroimaging tools that you plan to deploy in regional areas and what impact they will have?
Neuroimaging is a critical first step in distinguishing whether an ischaemic or haemorrhagic stroke has occurred in the patient. This distinction needs to take place before any further clinical decisions are made and proven effective treatment is applied. This is because the treatments are diametrically opposed depending on whether the patient has a blockage or a bleed.
In order to reach more Australians, we need ultra-lightweight, portable and cost-effective neuroimaging tools that can be deployed by standard rural ambulances and the Royal Flying Doctor Service. As it stands, the ASA has already delivered Australia’s first mobile stroke road ambulance, which Ambulance Victoria operates within a 20 km radius of the Royal Melbourne Hospital — it has cut treatment time by 41 minutes and treated 10 times as many patients in the first ‘golden hour’ after stroke. Our goal is to extend this emerging standard of care with a scalable imaging solution to the regional and remote areas of Australia, where over a third of our population resides.
Please describe the development process for EMVision’s portable brain scanner and how the technology works.
Our scanner is the brainchild (excuse the pun) of some of the brightest minds in electromagnetic imaging out of the University of Queensland. These researchers have spent the better part of a decade advancing imaging techniques. Our IP portfolio was originally developed by Professor Amin Abbosh and Professor Stuart Crozier alongside a team of approximately 30 researchers.
EMVision was subsequently founded to acquire this IP, commercialise the technology and in doing so, provide more accessible imaging to patients everywhere.
Our technology uses signals in the electromagnetic spectrum (non-ionising) to distinguish between ischaemic and haemorrhagic strokes in a matter of minutes. It acquires data in under 30 seconds and does not require any contrast agents. It’s also very light, portable and easy to use, meaning it’s faster, safer and more accessible for time-sensitive medical emergencies like stroke.
How will EMVision’s technology help to provide equal access to health care?
Today’s imaging technologies provide fantastic images but for the most part, they are heavy, immobile, expensive and require purpose-built rooms.
The goal with our technology is to help enable stroke diagnosis and care wherever the patient is, whether that’s by the bedside in a hospital, or in the future, out in the community or in an ambulance.
With the support of the ASA, we plan to test, validate and implement a new model of care across our country and in doing so, create a template for the implementation of innovative stroke care across the globe.
From vision to vigilance: building a secure digital future for health care
Digital health adoption offers clear benefits, yet Australians continue to scrutinise how their...
In Conversation with Australasian Institute of Digital Health CEO Anja Nikolic
Hospital + Healthcare speaks with Australasian Institute of Digital Health CEO Anja...
Cutting-edge digital health tools putting plastic, silicon and steel to the sword
The Australian Digital Health Agency's Chief Digital Officer sets out some sustainable...


![[New Zealand] Transform from Security Awareness to a Security Culture: A Vital Shift for SMB Healthcare — Webinar](https://d1v1e13ebw3o15.cloudfront.net/data/89856/wfmedia_thumb/..jpg)
![[Australia] Transform from Security Awareness to a Security Culture: A Vital Shift for SMB Healthcare — Webinar](https://d1v1e13ebw3o15.cloudfront.net/data/89855/wfmedia_thumb/..jpg)




