In Conversation with Bethan Richards, Australia's first CMWO

In Conversation provides a glimpse into the life on an ‘outlier’ — an exceptional person going above and beyond to innovate in their field and improve patient outcomes. This issue’s guest is Australia’s first-ever Chief Medical Wellness Officer (CMWO) at Sydney Local Health District (SLHD), Bethan Richards*.
Richards wears many hats. She is the Head of the Department of Rheumatology at Royal Prince Alfred (RPA) Hospital, Sydney, Deputy Director of the Institute for Musculoskeletal Health and Director, WellMD Centre, SLHD. In 2019, Richards was appointed as Australia’s first CMWO at SLHD to improve staff health and wellbeing, and reduce stress and burnout. Here she reflects on her journey so far and details how a staged, data-driven and collaborative, yet individualised, approach has improved outcomes.
How did the CMWO role come about?
Prior to becoming the Head of Department of Rheumatology at RPA, I was the network director of physician training. The job involved looking after the training and wellbeing of 60 basic physician trainees (BPTs).
After being in the role for five years, I noticed a significant increase in distress that seemed to be occurring in trainees each year. This meant I was spending more and more time counselling them and was referring larger numbers of trainees for formal external assistance. This, despite the fact that we were running a training program that was arguably the best in the country, with each trainee receiving formal mentorship.
In 2017, in a period of four months, four basic physician trainees (out of 400) in NSW took their own lives. This was shocking and heartbreaking — it led to a lot of grief, anger and reflection. Locally, it amplified the conversation regarding trainee wellbeing and efforts to better understand the factors influencing this.
At my health district, we had an initiative called ‘The Pitch’, where anyone could pitch an idea to the Chief Executive for $50,000. The trainees and my training team came together and designed a pilot wellbeing program called BPTOK. In 2017, we pitched the program successfully to Sydney Local Health District (SLHD) and ran the pilot over the next two years.
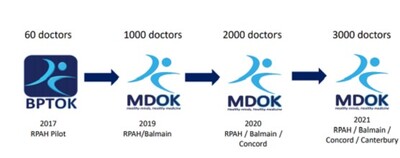
In 2018, NSW Health launched the JMO BeWell program to fund initiatives that addressed junior doctor wellbeing. We applied for funding to roll out BPTOK to all junior doctors in a three-year phased approach across the Sydney LHD (RPAH and Balmain hospitals in 2018/19, Concord in 2019/2020, Canterbury in 2020/21) as MDOK, and were successful in our grant for $210,000. We also realised the importance of addressing senior doctor wellbeing, so we opened up MDOK to all doctors working in the district.
In 2018 I went to Stanford University to learn what had been achieved in the US (there were no similar programs in Australia) and did the Chief Wellness Officers Course. Following my return, my Chief Executive created the first Chief Medical Wellness Officer position in the country. The role involved establishing the SLHD MDOK Wellbeing Center and creating a project team, establishing routine wellbeing measurement of medical officers at SLHD, and developing, piloting, evaluating and promoting medical officer wellbeing initiatives in the SLHD.

Tell us about the early days in the role.
Early days were tough. Emotions were high and wellbeing was not a topic that was openly discussed in the medical world for fear of being seen as ‘weak’ or ‘not coping’.
Convincing people to spend precious time on wellbeing skills and knowledge training was challenging, and there was a lack of understanding about what physician burnout was, why it mattered and what meaningful changes could be brought in.
At that time, there was no governance structure around wellbeing within the organisation. There was limited evidence to guide us and while many anecdotes and opinions were offered, there was no data to back them up. There was also pressure to help everyone all at once. Also, it became apparent early on that what stressed one doctor did not necessarily affect another, and conversely, if a wellbeing strategy helped one doctor, it did not mean it would help others.
A lot of the early days were spent collecting data and educating executives, junior and senior medical staff and their colleagues about what the problem was, why was it happening, why they should care about it and what it was proposed that we do about it.
What does the program involve?
MDOK is Sydney Local Health District’s multifaceted and evidence-based wellbeing program that is driving organisational, cultural and systemic change. The model developed and piloted in the RPA BPT cohort of 60 doctors has been successfully implemented at multiple facilities in the SLHD for around 3000 doctors. Components of MDOK have also been also adopted by various specialty societies and other craft groups. Please refer to Image 1 for our staged approach to the program:
Over the last four years, we have managed the delicate balance between running a resourced, sustainable and tailored program with the pressure of needing to address the wellbeing of greater numbers of doctors at all levels of their careers as well as the need to help address all staff wellbeing.
Over time, we have built MDOK around five key pillars of wellbeing (physical; psychological; social connection; leadership and performance; and culture and safety) as well as ensuring cultural and system-level interventions and use of a data-driven approach.
Each pillar has a series of tactics to address wellbeing, and to date, more than 200 initiatives have been piloted. In 2020/21 we had 56,302 measurable interactions with the MDOK program. This included 18,969 interactions with MDOK physical wellbeing initiatives, 27,633 interactions with psychological wellbeing initiatives, 3915 interactions with social wellbeing initiatives, 1159 interactions with leadership and performance initiatives, and 4626 interactions with culture and systems change initiatives.
COVID-19 created many challenges for the program. There were shifts in job roles, constant uncertainty and staff shortages, and the strict rules on isolation interfered with our ability to deliver many wellbeing activities face to face. We pivoted to the virtual world, which brought some benefits — there was increased engagement and flexibility to reach people, but at the expense of true human connection.
We had 3588 Zoom session attendances at the MDOK COVID-19 Education Series and 2010 hits for the MDOK initiatives hosted on our private YouTube site. With several initiatives targeting all staff and being difficult to measure the individual interaction with (eg, sparkling/still water fountains, #TheatreToastie, protected lunch break, R.E.S.E.T, on call room upgrade), it is likely that the true engagement of SLHD staff with MDOK initiatives is much higher than this.
Do staff do things differently because of MDOK?
Our data shows:
- Rates of doctors that have a GP have increased from 55% to 75%.
- Rates of doctors who have reached out for help to EAP or MDOK increased by 150%.
- Rates of sick leave in junior doctors increased (meaning they are not coming to work sick as was the historical culture). COVID has really helped this.
- Rates of doctors who have lunch has increased.
- Rates of doctors who drink water during the day has significantly increased.
- Lower rates of distress and burnout and higher rates of self-compassion and resilience in doctors who engage with MDOK activities.
- More frequently medical staff are sharing difficult experiences publicly, have check-ins and huddles built into workday practices.
- All orientation processes now include MDOK sessions, all junior doctors have specific MDOK sessions built into their training programs, MDOK is an agenda item on quality and safety committees, departmental committees, medical boards.
- Wellbeing measures are now a routine part of practice and measured yearly (ethics approved database created).
How critical is leadership in bringing change and improving wellbeing?
Absolutely critical. We have a pillar dedicated to this and executive and senior clinician buy-in is a must. Yet ironically, doctors receive no leadership training, and those in leadership positions have limited support. Our leaders are the guardians of the culture; to change the culture we must have our leaders engaged and role modelling the behaviours we are aspiring to. In health care work is delivered in teams and so leaders have a great sphere of influence on the wellbeing of medical and non-medical colleagues around them.
Wellbeing champions are a critical part to achieving a shift in culture on the issue of wellbeing in large organisations and can occur at any level. Dedicated leadership resources to address wellbeing and a governance structure that empowers these leaders to effect change are must-haves. There is good evidence for the positive effect of coaching in doctors that leads to a reduction in burnout and improvement in wellbeing levels.
Could you summarise key insights from the program journey?
Some of the key points included: staff wellbeing requires a data-driven approach; burnout is a quality and safety issue; there is no one solution to wellbeing/burnout so we need a menu of options; each department or hospital has different issues so we cannot use a ‘blender approach’; staff wellbeing should be a number one priority with dedicated resources allocated to it; we cannot address ‘all staff wellbeing’ without understanding the issues that affect different groups; instead of focusing on the individual, we must address the system and cultural issues; senior executive engagement is critical to effect, meaningful and sustainable change; solutions come from the front line; social connections enhance wellbeing.
After reviewing our model, the Australian Medical Association has recommended the appointment of a chief wellness officer in hospitals as part of its position statement on the health and wellbeing of doctors and medical students 2020. In 2021, NSW Health recommended the appointment of a chief wellness officer in its Staff Wellbeing Strategic plan.
Incontinence management innovations for healthcare facilities
Incontinence management is rapidly improving courtesy of new technologies and compassionate...
Remote laundries target preventable disease in NT communities
A new community laundry has launched in Borroloola, part of a program seeking to curb preventable...
Eye care partnership looks to support First Nations optometrists
A new scholarship initiative will support Aboriginal and/or Torres Strait Islander optometrists...



![[New Zealand] Transform from Security Awareness to a Security Culture: A Vital Shift for SMB Healthcare — Webinar](https://d1v1e13ebw3o15.cloudfront.net/data/89856/wfmedia_thumb/..jpg)
![[Australia] Transform from Security Awareness to a Security Culture: A Vital Shift for SMB Healthcare — Webinar](https://d1v1e13ebw3o15.cloudfront.net/data/89855/wfmedia_thumb/..jpg)




