Nurses better at identifying colorectal cancer
Nurses are at the forefront of identifying colorectal cancer, with superior outcomes to a physician-led model.
According to research published in the Medical Journal of Australia, a nurse-led model of colorectal cancer surveillance has improved compliance with guideline recommendations to 97%, reduced the number of unnecessary colonoscopies and reduced the number of cases progressing to cancer.
The early diagnosis of colorectal cancer (CRC) is vital and can be achieved with screening by faecal occult blood tests (FOBT) or colonoscopy, wrote the authors, led by Dr Erin Symonds, senior scientist for Flinders Medical Centre, based at the Flinders Centre for Innovation in Cancer, in Adelaide.
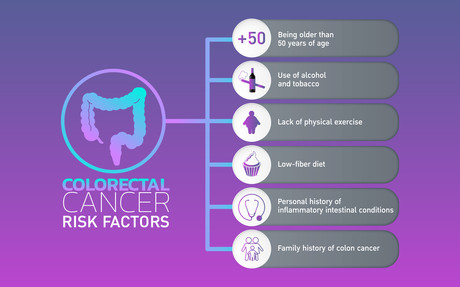
“A family of CRC or a personal history of adenoma can increase a person’s risk of CRC as much as fourfold, and such individuals are advised to undergo regular surveillance colonoscopy,” Symonds and colleagues wrote. “Screening and surveillance guidelines aim to optimise the effectiveness of CRC prevention, with surveillance intervals generally ranging between one and five years.”
Compliance with those recommendations is poor, however, with as many as 89% of patients receiving inappropriate surveillance, usually a colonoscopy before the recommended date. The Southern Co-operative Program for the Prevention of Colorectal Cancer (SCOOP) was established in 1999 to “improve surveillance rates to match the Australian National Health and Medical Research Council guidelines on CRC prevention”. After early success (compliance by 2000 had increased from 46% to 96%), SCOOP was expanded to use two models: one nurse-led in public academic hospitals, where nurses make recommendations based on NHMRC guidelines, which are then confirmed by a physician; and the other, physician-led in private non-academic hospitals where the specialist physician manages the entire process.
In the latest research, both models were audited over a 3-month period. In the nurse-led model, compliance with surveillance guidelines was achieved in 97.1% of cases, and in the physician-led model, compliance reached 83%, a statistically significant difference.
“Having a process in place that allows for long-term compliance with surveillance guidelines will promote optimal health care, as procedures performed too frequently can increase risks to patients, are expensive, and lengthen waiting lists,” Symonds and colleagues wrote.
“Continuous monitoring of and education about colonoscopy surveillance intervals for patients at elevated risk of CRC promotes adherence to recall guidelines and efficient use of limited endoscopy resources.”
Heart failure device could prevent hospitalisation
The device may be able to detect signs of fluid overload and could be used to monitor patients...
SJG Bendigo Hospital expands cardiac care service
The service has six cardiologists rostered onsite to provide diagnosis and treatment as part of...
WHO releases guidelines for catheter-related infections
Poor practices in the insertion, maintenance and removal of these catheters carry a high risk of...











