Human Factors and Safety Improvements for Infection Prevention
Wednesday, 21 September, 2016
There are around 200,000 healthcare-associated infections (HAIs) in Australian acute healthcare facilities each year. This makes HAIs the most common complication affecting patients in hospital. As well as causing unnecessary pain and suffering for patients and their families, these adverse events prolong hospital stays and are costly to the health system.1
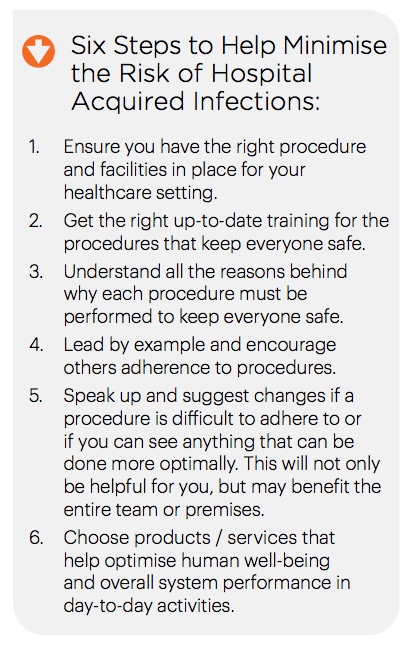
However, a significant number of these infections can be reduced or prevented and the first step, according to Professor Jane Reid, is introducing a safety culture in the hospital and healthcare setting and being more open to doing things ‘differently’.
Professor Jane Reid is a Registered Nurse, Researcher and Independent Healthcare Advisor with the NHS and a Non-Executive Director. Earlier this year, Professor Reid presented at the ACORN Conference on a topic she’s extremely passionate about - human factors and patient & staff safety. While she was in town, Professor Reid also presented to the Clinical Excellence Commission (New South Wales).
Infections can have serious consequences, especially in the most vulnerable of hospital patients. It can result in surgical wounds not healing and respiratory and urinary tract infections.2 These complications are not only dangerous for the patient but drain valuable healthcare resources.
What may be surprising however, is that at least half of healthcare associated infections are preventable.3 The science of Human Factors and Ergonomics and a positive Safety Culture can make a significant contribution.
Human Factors refers to environmental, organisational and job factors, and the human and individual characteristics which influence behaviour at work in a way that can affect health and safety.4
“People might know what is the right thing to do but whether they actually do it is another matter.”, said Professor Reid.
“The science of Human Factors has a lot to offer. Consider hospital acquired infections. We can consider the lapses that may have contributed to that infection – lapses in systems, lapses in processes and lapses in our attention. It invites us to look at the pathway of care and think about all of the elements that we need to put right to ensure that patients get the best care possible.”
“The greatest challenge to compliance with infection prevention measures is the concept of compliance itself,” says Professor Reid. “The way I view safety is that compliance is about good enough, and I don’t want good enough for my family, or my loved ones – I want excellence.”
“I would like the healthcare industry to get to a place where people understand that their individual contribution makes a huge difference. We also need to look at advances in technology that reduce the potential for harm – products like BD ChloraPrepTM cutaneous solution, which has been available in the UK since 2006, are helpful in reducing the incidence of infection.”
“Regularly when I’m working with clinical staff I talk about a pledge - a commitment to delivering the very best of care. We need to instil a passion and a sense of ‘not on my watch’. To ensure that we’re attentive to potential lapses and we absolutely commit to doing the right thing at the right time for every patient.”, Professor Reid concluded.

BD ChloraPrepTM is the trademark of Becton, Dickinson and Company. Learn more about the Difference of One at bd.com/AU-BDNew

Non-invasive 'virtual' biopsy for skin cancer diagnosis
Researchers have developed a new imaging method that allows clinicians to analyse the skin...
UTI vaccines could prevent infection for nine years
MV140 is a new vaccine for recurrent UTIs and is administered with two sprays of a...
What's the key to retaining rural GPs?
Understanding doctors' decisions to stay or leave, once recruited, could provide insights on...










